A Patient’s Guide to Hand Fractures with Animated Surgical Video
Introduction
Fractures of the hand are common injuries. A fracture implies a break of any of the bones of the hand. Typically, fractures are associated with trauma—a fall, motor vehicle accident, bicycle mishap or sporting event.
Due to the presence of multiple joints, hand fractures require skilled care. Fortunately, most hand fractures can heal without surgery. However, even fractures managed without surgery may require extensive bracing and therapy due to stiffness and swelling these injuries cause.
Anatomy
The hand is the terminal functional unit of the arm. It is connected to the arm via the forearm (radius and ulna) and the eight bones of the carpus the hand is composed of both metacarpal and phalangeal bones. These bones are the foundation for function of the four fingers and thumb.
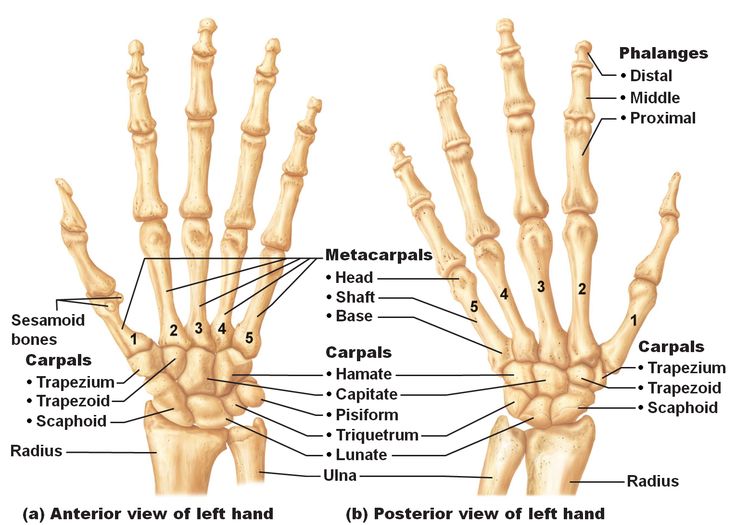
Bones of the hand and wrist from a front and bottom view.
Diagnosis
Symptoms
Almost all hand fractures occur as a course of trauma—the vast majority are due to falls on an ourstretched arm. Patients tyically report pain, swelling, deformity, and bruising of the hand. Inhibition of finger and wrist motion are also common complaints.

X-ray of a displaced fracture of the shaft of the 5th metacarpal bone.
Hand Surgeon Examination
Physical Examination
Your hand surgeon will review your symptoms and inquire as to any pertinent family or medical history. At this point an examination of the injured limb is undertaken. Inquiries are usually directed to ascertain the presence of other ipsilateral injuries either to the wrist, forearm, elbow or shoulder.
An examination of the extremity is then focused on a neurological exam—both sensory and nerve motor function. Also the vascular status of the hand and digits are reviewed to insure swelling has not embarrassed the vascular supply. Areas of tenderness to palpation may indicate potential fracture, contusion or sprain. Skin integrity over areas with suspected fracture are noted—as these areas may indicated an open fracture.
Range of motion of joints is reviewed—both potentially as passive and active range of motion. In fractures of the hand, motion can uncover alignment issues including splaying or scissoring of digits. For hand injuries, with the fingers flexed the nails typically point toward the scaphoid bone of the wrist. Abnormal rotation is again accentuated and better appreciated with range of motion of the hand.
Imaging
Plain x-rays are the workhorse of evaluation for hand fractures. Multiple angles may be necessary to uncover and appreciate fractures. Some hand and wrist fractures may not be discernable on initial x-rays. If there is suspicion of fracture, often the extremity is splinted and the patient recalled in 1-2 weeks for additional x-rays.

X-ray of a displaced fracture of the shaft of the 5th metacarpal bone.
Advance imaging such as CT or MRI is sometimes useful. CT offers the advantage of viewing complicated fractures from multiple viewpoints. Modern CT also offers the opportunity to do 3D reconstructions of injuries to provide enhanced viewing.
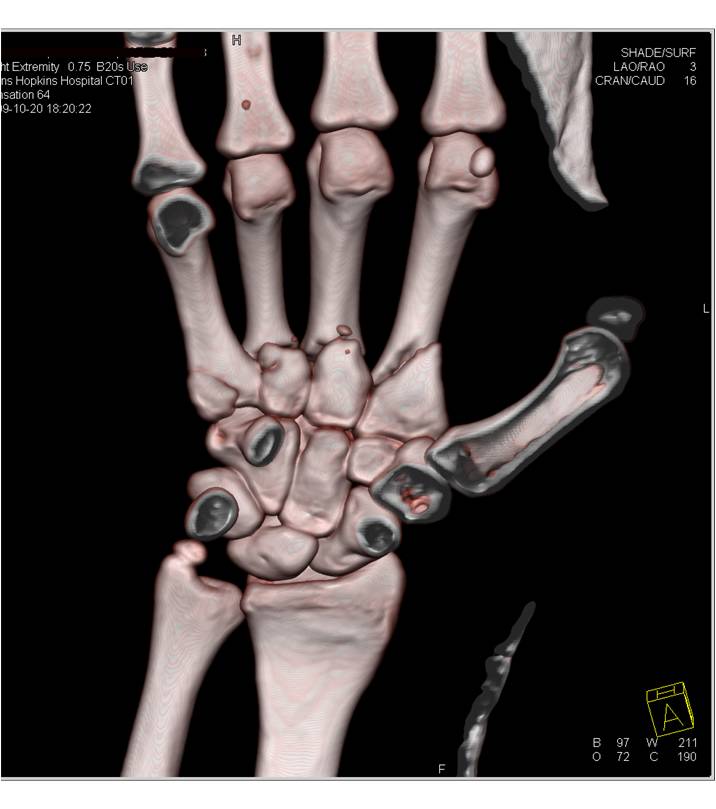
A 3 D CT scan showing displaced fractures of the base of the index, long and ring metacarpals.
MRI is best suited to add additional information regarding soft tissues injury associated with fracture. MRI offers the ability to image tendon, ligament and muscle.
Treatment
Nonoperative
The vast majority of hand fractures will respond to nonoperative management. Immobilization is typically the first step and the utilization of splints, casts or braces form the initial algorithm for treatment.
Immobilization is typically coupled with elevation to decrease swelling. Immobilization for hand injuries is specific for the injured area. Many times the immobilized position is termed an “intrinsic plus” position—in that the proximal finger joint is flexed 90 degrees while the distal joints are held in extension. Changes in immobilization as the fracture heals is typical and patients may progress through a variety of splints, casts, and braces.
Range of motion of an effected joints or areas prevents stiffness from becoming an issue in areas without fracture. Also the braces utilized for fracture typically becomes shorter as healing progresses. Involvement with hand therapy is typical for many hand fractures. A hand therapist can guide the balance between immobilization necessary for fracture heading—and motion necessary to limit joint stiffness.
Operative
Hand fractures with displacement or rotation may require surgical treatment. Surgery is aimed at restoring alignment and maintaining this alignment. Maintenance of alignment typically requires the placement of hardware into the hand.
Most hand fracture surgery can be completed as an outpatient surgery and the majority done under regional anesthesia. Hardware associated with fractures typically involves either pins (Kirschner wires) or specialized plates and screws. Because the bones of the hand are smaller, proportionately smaller pins and screws are necessary for fixation. Because of the specialized structure of the hand, hardware removal may be necessary.

A fracture of the ring metacarpal treated with plates and screws
WATCH AN ANIMATED SURGICAL VIDEO OF TREATING HAND FRACTURES
For most patients, blood loss is minimal and unless there are medical indications—prophylaxis for deep vein thrombosis is not necessary. Other risks of surgery are small and include infection, bone healing, tendon rupture, and stiffness.
Patients are placed into a splint after surgery and typically return in two weeks for suture removal. Patients who receive regional anesthesia report less pain after surgery, but all patients should follow instructions regarding pain medications to improve their postoperative experience. Once patients recover from the surgical pain of application of the hardware, most report considerable improvement in their overall hand discomfort.
Rehabilitation
After surgery patients are instructed in elevation of the extremity and work on range of motion for the digits not affected. At two weeks most patients have suture removal and some are placed into a removable brace… By six weeks after surgery, most patients will have considerable healing of the fracture will likely start weaning from the splint. Work on range of motion can be accomplished at home or with the help of a hand surgeon. Strengthening of the hand, wrist, and arm are emphasized and most patients should gain good use of their wrist and hand—especially with diligent work on motion and strength.
Outcomes
Modern fracture care has greatly improved the results for patients. However, patients can still expect some degree of stiffness with any fracture care and at times additional surgery may be warranted. Return to sports after injury typically requires 3-6 months. Patients report continuing improvement for up to one year after injury.