A Patient’s Guide to Shoulder
Fractures (Fractures of the
Proximal Humerus)
Introduction
Shoulder Fractures are among the most common breaks of the human skeleton. Fractures may occur at any of the bones which constitute the shoulder, but the clavicle (collarbone) is the most commonly injured. The second most common area injured in the shoulder is the proximal portion of the humerus. Fortunately, most fractures of the shoulder respond to treatment without surgery.
Anatomy
The shoulder serves as a connection between the chest and arm. The clavicle functions as a strut connected to the shoulder bone (scapula). The scapula articulates with the humerus and accounts for approximately 70% of shoulder motion (the remaining motion occurs between the scapula and the thorax). Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
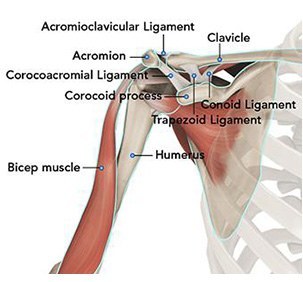
A right shoulder viewed from the front showing the clavicle, humerus and scapula.
The motion between the shoulder blade and scapula is a stable gliding surface over bursal structures and not prone to dislocation. However, the articulation between the humerus and scapula has little bony stability. This is because the ball of the humerus is large and the socket is small on the scapular side—think of the small amount of stability a golf ball has on a tee.
The inside layer of muscles gives the shoulder stability and motion above shoulder height and is called the rotator cuff—a series of 4 muscles
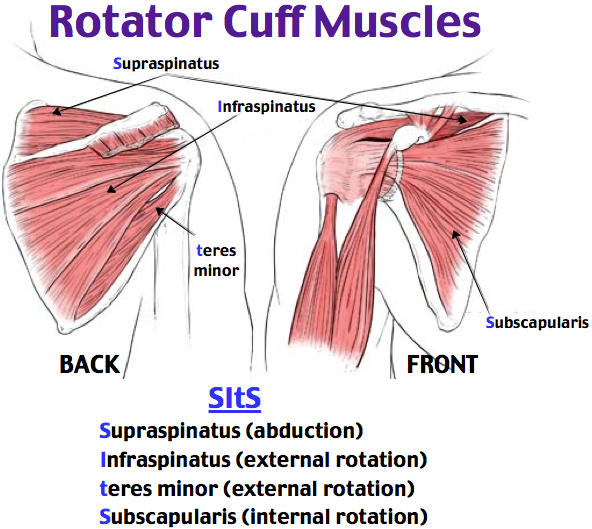
The muscles underlying the deltoid—the rotator cuff viewed from the back and front
Diagnosis
Symptoms
Patients with fractures of the shoulder complain of pain, bruising, and often deformity. The weight of gravity on the arm causes increased discomfort.
Surgeon Examination
After reviewing the patient’s symptoms, a review of their pertinent medical history and family history is obtained. The range of motion of the shoulder is measured in multiple planes. The strength of the shoulder in resisting motions is tested. The location of the deformity is determined and a neurologic and vascular exam of the extremity completed. Patients with shoulder fractures may have neurological dysfunction arising from nerve bruising at the time of injury
Imaging Studies
X-rays of the shoulder are typically utilized for evaluation. Although x-rays do not image the soft tissue of the rotator cuff, they can add information regarding the presence of arthritis, fracture or dislocation. Often x-rays may be the only study required for evaluating shoulder fractures.

A radiograph (x-ray) of a left shoulder demonstrating a fracture of the proximal humerus involving the surgical neck, greater tuberosity, and lesser tuberosity. These fractures are denoted as four part fractures in a Neer classification
Advanced imaging can add additional information in understanding the pattern of a fracture. CT examination is most often used as it gives better delineation of bone than MRI. MRI is utilized if suspicion of additional soft tissue is warranted.
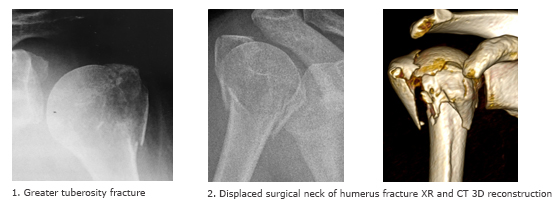
A routine frontal view of a fracture of the greater tuberosity in image 1. Image 2 shows the detail of a proximal humerus fracture comparing the routine x-ray and a 3D CT reconstruction.
Treatment
Nonoperative
As discussed in the image above, most shoulder fractures which are non-displaced or minimally displaced do not require surgery. These injuries are immobilized for comfort and once comfort is obtained a rehabilitation program is begun. Patients are instructed in range of motion and progress to add work on strength. These programs can often be performed at home. Recovery and return to sport varies but ranges from 8-16 weeks.
Operative Treatment
Displaced proximally humerus fractures may be candidates for surgical stabilization. In younger patients, plates and screws are the most common technique among many. In older patients, shoulder replacement, particular reverse shoulder, may be the treatment of choice.
WATCH AN ANIMATION VIDEO OF TREATING SHOULDER FRACTURES WITH PLATES & SCREWS

A displaced left proximal humerus fracture viewed from the front left image. Same shoulder after application of plates and screws and realignment of the fracture.
WATCH A VIDEO OF REVERSE SHOULDER REPLACEMENT FOR SHOULDER FRACTURE

A right shoulder proximal humerus fracture viewed from the front on the left image. The same shoulder after treatment for the fracture using a reverse shoulder prosthesis
Surgery is typically performed with a nerve block and supplemental anesthesia. Surgery typically requires less than two hours and the risks of blood transfusion are 1% in most studies. The need for medical prevention of deep vein clots after surgery is controversial and ranges from none, to aspirin, to mechanical compression to blood thinning agents. Other standard risks associated with surgery and arthroplasty are applicable to these types of procedures.
Rehabilitation
After surgery the arm is immobilized in a sling to allow for wound healing. Patients report pain after surgery, but the pain generally improves and the utilization of multimodal pain techniques have been shown to improve outcomes for patients. Night pain is typically the most problematic—but multimodal pain programs, heat, and sleeping elevated can improve this difficulty.
Many studies have shown that patients can successfully rehabilitate their shoulder on their own at home. Patients are typically guided through a therapy program and weaned from their sling over the first 8-12 weeks. Bone healing typically requires 6-10 weeks. Ingrowth of the tendon typically requires 4 months and patients, although direct ligament repair may occur somewhat sooner. Patients that continue to work on motion and strength show improvement for up to 1 year after surgery.
Dr. Groh is an expert shoulder surgeon
- Named top 60 Shoulder Surgeon in the USA by Becker’s Orthopedics
- Active member of the American Shoulder and Elbow Surgeons
- Written 50 Articles and Textbooks on Shoulder Injuries
- Holds patents and developed multiple shoulder implants and devices